Touch is the area that sent off the biggest alarm bells for us that our son had Sensory Processing Disorder. I say us it was the Pediatrician who first noticed it, as we struggled to peel him from stroking her shiny tights. We had completely missed the fact that he loved to cover himself in paint, and stroke people’s faces – we just thought that it was his age.
Touch is the area that sent off the biggest alarm bells for us that our son had Sensory Processing Disorder. I say us it was the Pediatrician who first noticed it, as we struggled to peel him from stroking her shiny tights. We had completely missed the fact that he loved to cover himself in paint, and stroke people’s faces – we just thought that it was his age.
Sensory Processing Disorder is when the information we constantly received by the seven senses is misinterpreted by the brain when it is processed. Sometimes our brains say there is TOO MUCH information coming in, and sometimes NOT ENOUGH. One of the areas this happens in is that of the Tactile sense – or touch.
Does your Child have Sensory Processing Disorder problems in the Tactile Sense (Touch)?
They may have problems with too much, too little or a mix of the two.
Signs of Too Much
Avoiding Touch
• Going barefoot, especially in sand or on grass, wearing sunscreen, hats, messy play with hands & feet (sand, mud, finger-paint). We often find a compromise of letting him wear sandals (no socks) even in Winter helps. Look out for any tags or labels on clothing/ hats that might bother them. Consider types of fabrics most preferred by the child. Use natural fibres e.g. cotton. Wash clothing before wear. Seam-less socks & underwear brands: online www.sensorydirect.com; or http://www.fledglings.org.uk sensorysmart.co.uk
• They become distressed during hair-brushing or cutting (our son was actually physically sick when he felt the hair fall and touch his skin. He is getting better but it is usually a case of one parent restraining him whilst the other just gets on with it (shaving in the case of hair). Allow the child as much control & independence as possible (e.g. control force & duration of own tooth-brush). Give warning prior to a disliked activity & talk them through it. Let them know how long until activity is finished (e.g. brush hair for the length of a favourite song/ use a timer set for 1 minute). Touch FIRMLY but gently. Light touch= startling. FIRM touch= calming. Always approach from the front. Warn them before you touch them. Use mirrors (e.g. hair-brushing, cutting, nail cutting, teeth brushing) so the child can see what is happening & increase control. The brushing technique helps with personal grooming. Avoid fans or vents blowing directly on child.
•  They use finger-tips instead of their whole hand. Give opportunities to play but without their hands e.g. touch play-dough/ paint with a brush/ spoon etc. before fingers. Slowly build them up – ie just started with finger-tips, then fingers, and reward them for trying it. Even let them play with their food.
They use finger-tips instead of their whole hand. Give opportunities to play but without their hands e.g. touch play-dough/ paint with a brush/ spoon etc. before fingers. Slowly build them up – ie just started with finger-tips, then fingers, and reward them for trying it. Even let them play with their food.
• They complain of being poked or bumped (this was common for both my oldest and youngest not understanding how much pressure people had used when touching them). They over-react to touch – e.g. lashes out. They avoid standing in line or close to others. They walk on their toes. They prefer to be in a protected place e.g. in a corner/ under a table. Pair them with a child that won’t prod or poke them. Have designated spots on the mat (e.g. carpet squares).Get the child to be the line starter/ ender/ hold the door.
Not Enough – The Sensory Seeker
• They touch people & objects to the point of irritating them (our Sensory Seeker is forever holding people’s faces in his hands).
They touch people & objects to the point of irritating them (our Sensory Seeker is forever holding people’s faces in his hands).
• They like people to touch him/ her (fantastic for cuddles).
• They are constantly touching other people’s hair or clothing (or just general touching – good idea to carry wipes. Do you have any idea how dirty the Tube is in London Underground but he HAD to touch it, then he didn’t want the black all over his hands and tried to rub it off on a stranger!!!!)
• They love to be barefoot (barefoot trails are just heaven).
• They pinch, bites, or hurts self (and/or others).
• They have a really high pain & temperature threshold.
• They hit or bang their head on purpose.
• They throw themselves on the ground.
• They enjoy rough play.
 How to Help
How to Help
• Allow them to fiddle with something that is appropriate & doesn’t distract others e.g. a pasta necklace/ bracelet; elastic necklace/ something with resistance. We have tags at the end of his weighted blanket. Allow a fidget toy in their pocket during seated time (e.g. car rides, mat time). *May need a social story to teach rules of use. Provide a squeeze/ stress ball for times that may be difficult.
• Be specific with words- “if you want to touch something- you touch …. Bracelet/ squeeze ball etc. so they have an alternative to their behaviour.
• Select highly textured clothing & lots of accessories e.g. head-bands, wrist-bands, belts.
•  Provide textured blankets or sheets for sleeping. We have surrounded him with teddies in his bed to aid night times as he was waking a lot and kept getting in or bed. But there he would really annoy us. There’s no other way to describe it – tickling, even scratching and kicking us – just really needing to get some sort of sensory touch input from us.
Provide textured blankets or sheets for sleeping. We have surrounded him with teddies in his bed to aid night times as he was waking a lot and kept getting in or bed. But there he would really annoy us. There’s no other way to describe it – tickling, even scratching and kicking us – just really needing to get some sort of sensory touch input from us.
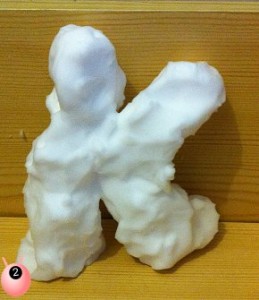
• Give opportunities to learn through touch experiences e.g. sand play, water play, messy play, finger-paints. Add textures to toy surfaces e.g. sand in finger-paints.
Many thanks to the Children’s Occupational Therapy Gloucestershire Care Services NHS Trust for supply this information and granting me permission to use it. This post is a redraft of a post previously published on Pinkoddy.